Discover our research, insights, and client successes to help you navigate change and accelerate value creation
Featured Insights
AI’s Tangible Impact on the Automotive Industry Explained

Featured Insights
Telecom API Market: The Whys and Hows
Featured Insights
Retail Hyper-Personalized AI Assistants Decoded

Featured Insights
How Is Manufacturing on Data-Rich Platforms Different?

Featured Insights
Limitations of AI in Quality Assurance
Featured Insights
Press Release

Featured Insights
How to Generate Value with Data Monetization in Telecom

Featured Insights
The Evolution of Quality Assurance: How AI is Changing the Testing Game

Featured Insights
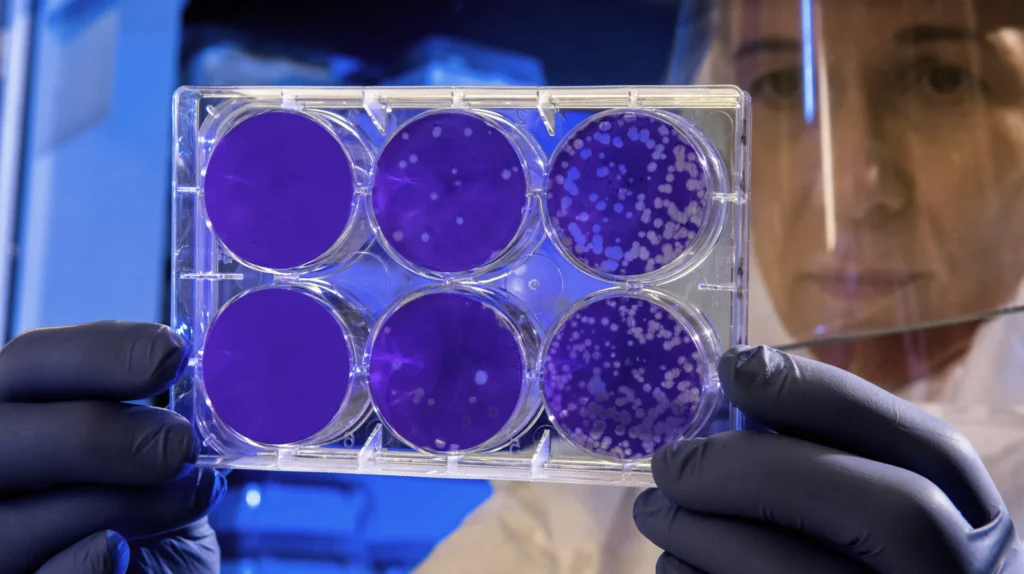
The Importance of Efficient Data Governance in Clinical Trials

Featured Insights
Press Release

Featured Insights
The Future of OSS/BSS in the Modern Telco Space

Featured Insights
Press release

Featured Insights
Microsoft Power Automate: How To Use Cloud Flows for Process Automation

Featured Insights
What Is Azure Key Vault? A Beginner’s Guide and Use Cases

Featured Insights
Generic API or Back-End for Front-End? You Can Have Both

Featured Insights
Machine Learning Research Problems
Featured Insights
Satellite Technology In 2025 And Beyond: The Future of GEO – Avenga