Technologies For Fraud Detection In Healthcare And The Pharmaceutical Industry
May 7, 2025 15 min read
Technologies stand at the forefront of fraud detection in healthcare and pharma which establishes more secure processes leading to better patient outcomes.
According to this report, healthcare spending in the United States alone is growing an average of 2.7% per year and is currently reaching $4.3 trillion. Within the skyrocketing healthcare expenditures, a major chunk of the funds is lost to fraud. Insights from the National Health Care Anti-Fraud Association (NHCAA) indicate the financial losses associated with healthcare fraud stand at about $300 billion. Keeping that in mind, finding a solution in the form of effective fraud detection in healthcare can help redirect billions of dollars, from covering fraud-related losses to improving patient outcomes.
Within this context, it is crucial to explore the different types of healthcare and pharmaceutical fraud in order to get an in-depth understanding of the topic in question. These insights illustrate the scope of the issue at hand and indicate the challenges the industry faces. The rest of this piece portrays the potency of the current technological tools that healthcare and pharma professionals use for fraud detection and prevention. So, it is time to plunge into the topic.
Types Of Healthcare And Pharmaceutical Fraud
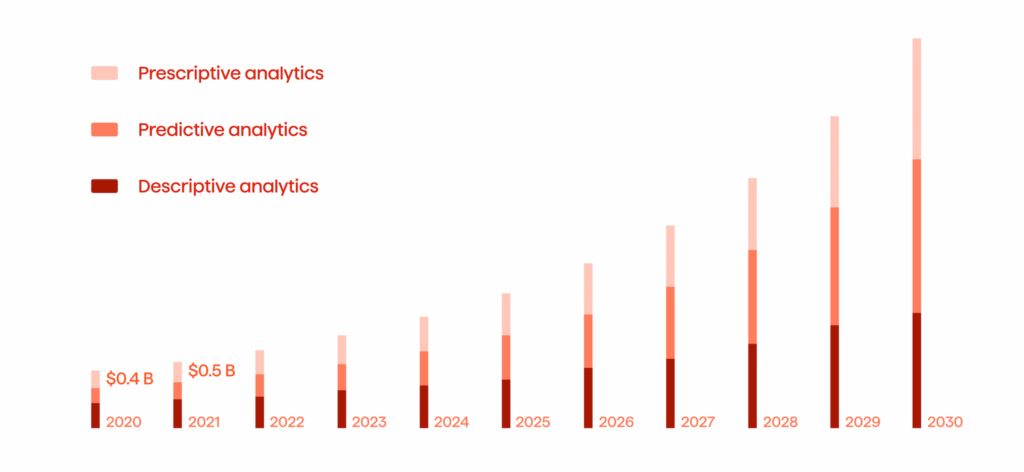
In the era of ongoing healthcare and pharma digitization, providers and organizations are facing the massive challenge of rising levels of fraud in various shapes and sizes. This means two things. First, fraudulent claims cost healthcare providers millions and even billions of dollars. Second, there is a rising demand for fraud analytics tools for fraud detection in healthcare (see Fig. 1).
Currently, the largest fraud-related settlement cost the pharmaceutical company Biogen a staggering $843 million. Yet, to understand the overall scale of the picture of healthcare and pharmaceutical fraud, it is crucial to focus on four key areas: fraud committed by medical providers, fraud committed by patients, fraud involving prescriptions, and fraud in pharma.
Fraud Committed By Medical Providers
When it comes to fraud originating from medical professionals and providers, we should talk about these particular types:
- Double billing. This healthcare fraudulent practice involves medical providers submitting different claims for the same procedure or service. In these cases, a medical professional tries to charge for multiple services while providing only one particular service. To illustrate, imagine a healthcare provider performing a single laboratory blood test for a patient. However, when presenting billing, a medical provider submits several separate claims for the same test. As a result, the insurance company might experience financial losses by paying the medical professionals twice. From a general perspective, double billing increases healthcare costs for everyone.
- Phantom billing. With this type of healthcare fraud, a medical provider charges for services or procedures that were never completed. In turn, the activity might also involve charging a higher price for a service that should cost much less. As an example, consider a healthcare provider billing an insurance company for a complex and costly surgical procedure that was never performed on the patient. In addition, medical professionals may charge for some brand-name medication while issuing less expensive generic versions.
- Unbundling. This practice encompasses billing for services separately while they should be billed together at a discounted rate. Most often, this healthcare fraud is committed to inflate the initial cost and to get a higher reimbursement from an insurance company. For instance, a medical provider might perform a series of related procedures on a patient. These are usually billed in a single package and come with a discount. Yet, the healthcare provider unbundles these procedures and submit a separate claim for each one while also charging the full price.
- Upcoding. This fraudulent activity involves medical providers charging for more expensive services and procedures than the patient actually received. With upcoding, a healthcare provider might perform a routine patient checkup, however, when issuing a bill to the insurance company, the medical provider charges as if a comprehensive examination was conducted.
Keeping the above types of healthcare fraud in mind, they involve medical providers committing the fraud and insurance companies being the targets of the fraud. As a result, the deceptive practices outlined above lead to higher cost of healthcare, something that will directly affect the patients as well.
Fraud Committed By Patients And Other Individuals
This next phenomena of fraud detection in healthcare addresses fraud committed by patients and other individuals. Respectively, we can list three types of fraud:
1. Bogus marketing. In the context of healthcare, bogus marketing means engaging in deceptive practices that are performed to get a person’s health insurance identification number as well as PHI (Protected Healthcare Information). This practice often involves enrolling a patient in a fake benefit plan or by billing for services that never occurred. To illustrate, scammers might use bogus marketing by posing as a healthcare company representative. This person often calls unsuspecting people and convinces them to provide their health insurance ID numbers and PHI. Later, the scammer will use the information to submit false claims or to enroll that person in a fraudulent health plan. Overall, bogus marketing is on the rise and a part of the growing digital advertising fraud phenomenon which currently is costing about $81 billion.
2. Identity theft and identity swapping. This type of healthcare fraud includes using someone else’s health insurance data without that person knowing. Often, identity theft takes place via situations of unauthorized access to health information as well as data breaches. In this case, this type of fraud leads to financial losses for patients and insurance providers. For example, consider a person without health insurance borrowing or stealing someone else’s insurance card in order to get medical treatment. This leads to false information in medical records and higher insurance premiums for the policyholder.
3. Impersonating a healthcare professional. The final type of healthcare fraud in this segment is the impersonation of a healthcare professional. This imposter bills for health services and equipment without a medical license. People using this type of fraud might pose as nurses, doctors, and other medical professionals. Notably, with tools like ChatGPT that are currently unregulated, these criminals can use potent tech tools to aid in their impersonations. Sometimes, a person might even set up a fake clinic and claim to be a licensed physician. Without proper fraud detection healthcare tools, it would be hard to verify whether a claim for a service or procedure is issued by a licensed professional or just someone posing as one.
While fraud committed by medical professionals is mostly directed against insurance companies, this type of healthcare fraud is mostly directed against patients. As a result, people can experience financial losses, loss of sensitive information, and data theft.
Fraud Involving Prescriptions
When digging deeper into healthcare fraudulent activities, it is important to speak about fraud that involves prescriptions. This fraud type stands on the boundary between healthcare and pharmaceutical fraud. Now, let’s discuss prescription fraud:
- Forgery. It is estimated that pharmacy fraud is responsible for at least 1% of all pharmacy costs, which is about $358 billion. In this context, forgery is a major driver behind this fraud phenomenon. This fraudulent activity encompasses altering or creating a prescription without proper authorization. Additionally, forgery can also mean completely falsifying a medical prescription. Patients and medical professionals alike can commit forgery.
- Diversion. This type of pharmacy fraud involves diverting legal prescriptions for illegal uses. Essentially, it means the prescribed medications are redirected from their initially intended and legal use to an illegal one through unauthorized channels. To illustrate, a pharmacy technician might steal medications from the inventory and sell them on the side. In turn, a patient with a legitimate condition gets legally prescribed controlled substances and then sells them to third parties.
- Doctor shopping. Finally, this type of healthcare fraud entails a person visiting multiple medical providers or hospitals to get prescriptions for controlled substances that are later resold or used above the prescribed dosage. Doctor shopping is usually done within a short time frame. A person with an opioid addiction might visit multiple doctors in a single month and try to obtain prescriptions for opioids, stimulants, and/or benzodiazepines. Later, this person uses these controlled substances to support their personal addiction or sells them on the black market.
All in all, fraud involving prescriptions is big. It involves a lot of money made illegally through medical prescriptions forged or misappropriated. Subsequently, while being on the boundary of healthcare and pharmacy fraud, dealing with counterfeit prescriptions is something that can cause serious harm to people, as well as cause reputational damage to pharmacies.
Fraud In Pharma
Last but not least, there is simply pharmaceutical fraud. Proper healthcare fraud detection involves dealing with the massive scope of pharma-related fraud. Because of this problem’s scope, there are at least eight types of this fraud:
1. Kickbacks. These are illegal payments offered by pharma companies to medical professionals or individual pharmacists in exchange for particular drug promotions. Kickbacks lead to biased decisions, thus affecting the quality of patient care. For instance, several years ago Insys Therapeutics, an opioid manufacturer, was found guilty of offering kickbacks to healthcare professionals who prescribed the manufacturer’s fentanyl-based painkiller.
2. Off-label marketing. This pharmaceutical fraud includes promoting pharma products not approved or regulated by the FDA. Off-label marketing is dangerous and can result in people taking these drugs only to discover some serious and/or undocumented side effects.
3. Billing for the brand. This practice encompasses charging governmental healthcare programs for particular brand-name medications while cheaper and more generic alternatives are available. Billing for brands leads to healthcare professionals, insurance companies, and patients paying more when they could have paid less. Moreover, this type of pharmaceutical fraud is directly related to phantom billing, a type of healthcare fraud mentioned previously.
4. Best price fraud. This fraudulent activity occurs when a pharma company misrepresents the product price when working with programs like Medicaid. Best price fraud is purely motivated by profit maximization. While legally defined as a white-collar crime, there are numerous examples when major pharma companies engaged in this practice. Perhaps, the most prominent example occurred with TAP Pharmaceuticals Products Inc., who paid $875 million for inflating the prices for Lupron, a prostate cancer drug.
5. Current Good Manufacturing Practice (CGMP) violations. CGMP ensures that pharma products follow quality standards within each step of the production process and supply chain. When pharma companies fail to adhere to CGMP regulations, it leads to defective and contaminated products. This could potentially cause harm to end-users.
6. Medicaid price reporting fraud. This type of pharmaceutical fraud includes pharma companies providing false pricing information to the Medicaid program. It results in increased reimbursement and higher healthcare costs. The biggest case of this occurred with Pfizer. In 2009, the company paid $2.3 billion for providing false information about several of its drugs.
7. Continuing Medical Education (CME) fraud. This type of fraud entails pharma companies using educational programs to promote their products. This practice creates bias among soon-to-be medical professionals, especially when it comes to choosing the best prescription(s) for their patients. To illustrate, in 2016 Warner Chilcott, a major pharmaceutical company, was fined $125 million for paying doctors who sponsored misleading CEM programs to promote the company’s drugs.
8. Manufactured compound drug fraud. Finally, here is a type of pharmaceutical fraud that encompasses pharma companies manipulating or altering drug compositions or pricing of combined medications. These are often custom-made medications for patients with specific conditions. In these cases, the parties involved in this type of fraud try to maximize profits from distinct and rare conditions.
The pharmaceutical frauds outlined above involve pharma companies trying to manipulate various drug production, distribution, and pricing processes for profit maximization. This is a corporate crime that can result in patients being exposed to contaminated, unverified, and unapproved drugs.
AI-Based Technologies Serving As Healthcare Fraud Detection
After covering the multiple types of healthcare and pharmaceutical fraud, it’s time to speak about fraud detection healthcare measures. In general, technological tools, like Artificial Intelligence (AI), have already proven themselves to be worthwhile when it comes to mitigating risks, addressing fraudulent activities, and anticipating errors. AI in the healthcare market is booming, yet despite that, there is an even greater need for AI-based fraud detection in healthcare than ever before (see Fig. 2).

Currently, fraud detection technologies have made massive breakthroughs. It is all fueled by data-driven innovations in cloud computing, data mining, Machine Learning (ML), and data analytics. These are all parts of the AI prodigy. When used correctly, they serve as effective fraud detection and prevention mechanisms.
Learn more about how we used AI-powered tools to boost the fraud detection capabilities for a global leader in embedded insurance. Success story
Now, it is time to understand how fraud prevention in healthcare actually works. The basic mechanism involves teaching AI how to engage in fraud detection procedures. This comes with the following steps:
1. Experts standing behind the AI-tool set specific rules and establish control over them.
2. Data analytics mechanisms are automated, anomalies are flagged, and all decisions are supported by a human data-driven approach.
3. An AI-tool learns from data sets and improves its fraud detection capabilities.
4. The next step is to double-check the flagged anomalies in order to distinguish between simple mistakes and fraud-backed anomalies.
With this basic understanding of the fraud detection mechanism, it is possible to develop an AI-tool that is comprehensive enough to detect even the most minimal traces of fraud. However, when speaking of measures to prevent fraud in heatlhcare in the first place, the following technologies can also be implemented:
1. Predictive modeling that uses predictive analytics, data mining, and quantitative analysis to detect fraudulent patterns in their germination stages.
2. AI-based pattern recognition to automate the process of detecting billing errors, which can help prevent a majority of the fraud committed by medical professionals.
3. Biometrics recognition includes iris scanners, facial recognition, and fingerprint scanning so as to improve and secure the patient identification process.
At the moment, the use of big data and AI is helping to push forward innovative fraud detection healthcare mechanisms. The power of ML and deep learning that come along with AI help provide a holistic view of interdependencies within a network under investigation. In simpler words, AI-based tools can help make sense of a myriad of healthcare-related data so as to recognize the patterns defined as fraudulent activities. Equipped with these tools, there is a higher chance to detect and prevent fraud in healthcare and pharma before any substantial damage is done.
Outcomes Of Tech Interventions Against Healthcare Fraud
Introducing AI-based fraud detection into healthcare and pharma is a great way to reap these benefits:
– Reduced time that healthcare staff members need to invest in processing data and doing manual tasks. A hospital can adopt an AI-powered system to automatically go through patient records to flag potential fraudulent activities like double billing, unbundling, and upcoding. Respectively, with such a system in place, staff do not need to go through the records manually.
– Higher rate of real-time fraud detection. AI-based tools analyze data in real time. In doing so, fraudulent patterns and suspicious activities can be detected in real-time. As a result, an organization employing the tool can take immediate action to deal with the fraud at hand.
– Saving costs and reputation. This is an obvious advantage. Considering all the financial losses due to healthcare and pharmaceutical fraud, implementing AI-based technology saves the money associated with all the resources spent on legal proceedings, reimbursement of fraudulent claims, and internal investigations. Besides, by having effective fraud detection measures installed, an organization protects itself from potential reputational damages. And, it also leads to a more secure and trustworthy environment being created.
Overall, the advantages of AI-based fraud detection in healthcare are numerous. From a higher degree of automation to a preserved reputation, the more protected you are against fraud, the lower the chance of fraud-related issues occurring.
Concluding Remarks
The alarming growth rate of data in healthcare makes it even harder to fight fraud. However, when appealing to AI tools grounded in big data, ML, deep learning, and predictive analytics, data can actually work for the benefit of the parties involved. Tech instruments can learn from the data and flag fraudulent activities as soon as they occur. Therefore, currently fraud detection in healthcare is a must, and there is not a single company operating in the industry that can afford to avoid their use.
When working with AI-based fraud detection, one needs to adopt the correct operational results. Moreover, with the growing complexity of fraudulent activities and more data being generated, it is also important to constantly review and adjust patterns at the core of any fraud detection mechanisms.
In any given scenario, please feel free to contact us and our expert teams can show you how to have top-notch and up-to-date fraud detection healthcare mechanisms in place.



